“I feel like my appetite is out of control”, “I can’t seem to lose weight”, “I’m gaining weight around my stomach and I have absolutely no energy”.
These are common complaints from clients struggling with high insulin levels or insulin resistance. Insulin resistance (IR). IR has become increasingly more common and is closely linked to other conditions such as PCOS (polycystic ovarian syndrome), type 2 diabetes, hypertension, and obesity. But what exactly is IR and how can we prevent and combat it?
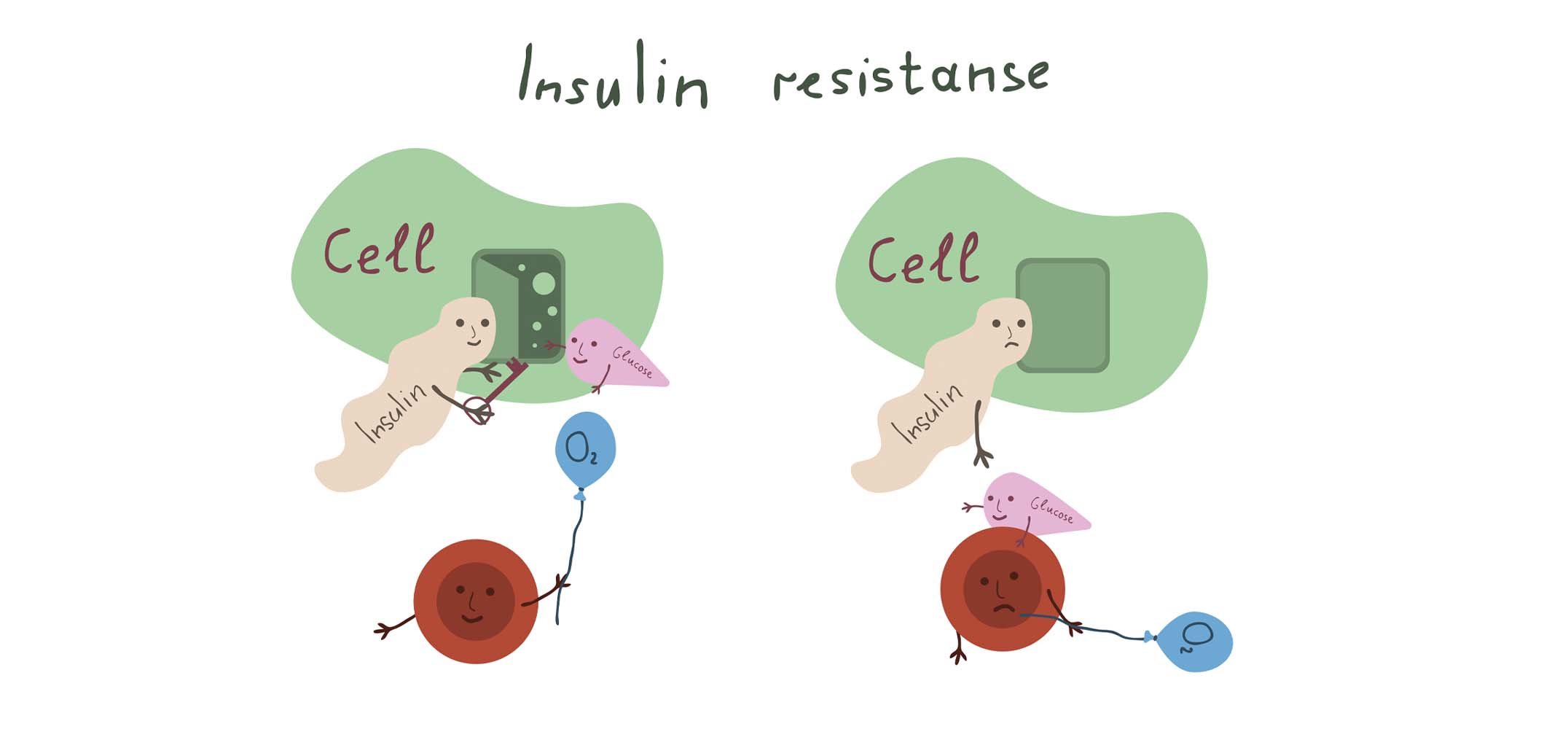
Insulin is a hormone in our body that acts like a key in our bloodstream, “opening” our cells to allow glucose to enter from the bloodstream. When we become insulin resistant, you can imagine the “insulin key” becoming a bit less effective or rusty and if we can’t open up our cells to let the glucose through- it will result in high blood glucose levels. This isn’t ideal, as high blood sugar levels can increase your risk for type 2 diabetes, hypertension, heart disease and inflammatory diseases.
Diet
Diet is the cornerstone of managing insulin resistance and irregular glucose metabolism. Focus on fiber-rich fruits and vegetables, lean proteins like chicken and fish, and healthy fats from nuts and olive oil. On the other hand, limit foods or become more mindful of your intake of refined sugars, processed carbohydrates, and unhealthy fats- as these groups can worsen insulin resistance.
There are many factors to look at in diet to assist with IR.
- The timing and composition of your meals can significantly impact your blood sugar levels and insulin sensitivity. According to literature, eating most of your calories and carbohydrates earlier in the day, particularly at lunchtime and in the early afternoon—can help keep post-meal blood sugar levels stable, as it has also been shown to be beneficial to avoid eating late at night.
- The order in which you eat different types of foods during a meal is also important. Starting with high-fibre foods such as vegetables, salads, or soups, followed by protein, and then consuming starchy foods last, can help improve blood sugar and insulin responses. An analogy for this would be to imagine a sink. The water from the tap is our sugar coming into the body, the drain-our cells and bloodstream. If we add soil to the sink (think high fibre foods, fats, proteins), the amount of time it takes the sugar to reach the drain (or our bloodstream) is greatly reduced. Resulting in lower absorption of glucose, and better insulin response.
- Another important factor is the glycemic index of our foods. The glycemic index (GI) of foods is influenced by the total carbohydrates in a meal, cooking methods, other macronutrients, and individual digestion. Aim for whole foods and avoid large quantities of quick-absorbing carbs like refined flours or starches, opting instead for resistant starches.
- Additionally, losing weight is a key strategy in treating insulin resistance, as it directly improves the body’s ability to use insulin effectively. Studies show that even 5-10% reduction in body weight is enough to make a remarkable difference in your insulin resistance.
- Diets like the Mediterranean diet, keto diet, low glycemic diet, and plant-based diet show promising effects in treating insulin resistance. Though, more studies are needed to determine whether it’s the weight loss or the diet composition that plays the biggest role. Alongside diet, aim for at least 150 minutes of moderate-intensity exercise weekly to help combat insulin resistance.
Supplements
Research shows that certain supplements can support insulin resistance management Our focus here is on the Sally-Ann Creed Berberine complex. Berberine helps lower blood sugar by promoting insulin secretion and increasing insulin sensitivity. Our complex also includes chromium, vitamin Bs, milk thistle, and probiotics like Lactobacillus acidophilus and Bifidobacterium species, which have shown modest but significant effects on reducing fasting blood glucose and HbA1c levels.
Blood Results
A few blood tests can provide insights into your insulin and sugar levels:
- HbA1c: Average blood sugar level over the past 2-3 months.
- Fasting Glucose: Blood sugar level after 8-12 hours without food.
- OGTT: Assesses how your body processes glucose over two hours after a fasting period and consuming a glucose solution.
- Fasting Insulin: Insulin level after fasting for 8-12 hours.
- Quicki Index: A calculation that assesses insulin sensitivity.
Managing insulin resistance might seem overwhelming, but with the right knowledge and lifestyle changes, it’s entirely possible to take control of your health. If you’re feeling uncertain about where to start or need personalized guidance, don’t hesitate to reach out. Our team is here to support you on your journey to better health.
Ogbu IS, Jane EO, Obeagu E. Insulin Resistance: A Review. 2024;2:11-28.
Papakonstantinou E, Oikonomou C, Nychas G, Dimitriadis GD. Effects of Diet, Lifestyle, Chrononutrition and Alternative Dietary Interventions on Postprandial Glycemia and Insulin Resistance. Nutrients. 2022;14(4):823. doi: 10.3390/nu14040823.
Foley PJ. Effect of low carbohydrate diets on insulin resistance and the metabolic syndrome. Curr Opin Endocrinol Diabetes Obes. 2021;28(5):463-468. doi: 10.1097/MED.0000000000000659.
Tabeshpour J, Imenshahidi M, Hosseinzadeh H. A review of the effects of Berberis vulgaris and its major component, berberine, in metabolic syndrome. Iran J Basic Med Sci. 2017;20:557-568.
Cao C, Su M. Effects of berberine on glucose-lipid metabolism, inflammatory factors and insulin resistance in patients with metabolic syndrome. Exp Ther Med. 2019;17(4):3009-3014. doi: 10.3892/etm.2019.7295.
Cao DX, Wong EY, Vela MN, Le QT. Effect of Probiotic Supplementation on Glycemic Outcomes in Patients with Abnormal Glucose Metabolism: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Ann Nutr Metab. 2021;77:251-261.
Fong C, Alesi S, Mousa A, et al. Efficacy and Safety of Nutrient Supplements for Glycaemic Control and Insulin Resistance in Type 2 Diabetes: An Umbrella Review and Hierarchical Evidence Synthesis. Nutrients. 2022;14(11):2295. Published 2022 May 30. doi:10.3390/nu14112295